Hi, everyone. Back in January I was having some gastrointestinal issues (blood, diarrhea, etc) so I went to the gastroenterologist and he ran some tests and said it was gluten sensitivity. I've been on a gluten-free diet for the past 6 months but the symptoms weren't getting better. Today I had a colonoscopy and it showed mild ulcerative colitis (proctitis/proctosigmoiditis).... I'm relieved I got a diagnosis but also concerned about what this means for my future. I don't want to take medication my whole life. I have two small children and the idea of having health problems scares me so much ;((( Does anyone on here have this disease or any advice on how to manage it? Thank you.
-
Planning tools
Get the WeddingWire app
Plan your wedding wherever and whenever you want on the WeddingWire app.Wedding guests Share with your guests to collect your wedding photos - Venues
-
Vendors
Complete your wedding team
Destination Weddings
Easily plan your international wedding.2024 Couples' Choice Awards
Check out this year’s best local pros, rated by couples like you. -
Forums
Stay up to date
- Dresses
-
Ideas
![Real Weddings]()
Real Weddings Find wedding inspiration that fits your style with photos from real couples
![Honeymoons]()
Honeymoons Sit back and relax with travel info + exclusive deals for the hottest honeymoon destinations
-
Registry
Create your all-in-one registry Find a couple's WeddingWire RegistryFeatured registry brands See all registry brands
- Wedding Website
-
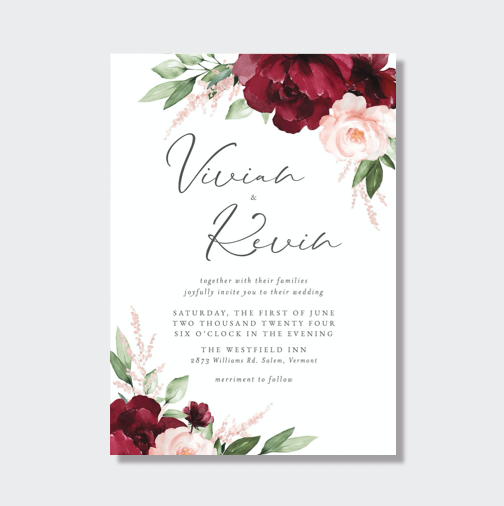
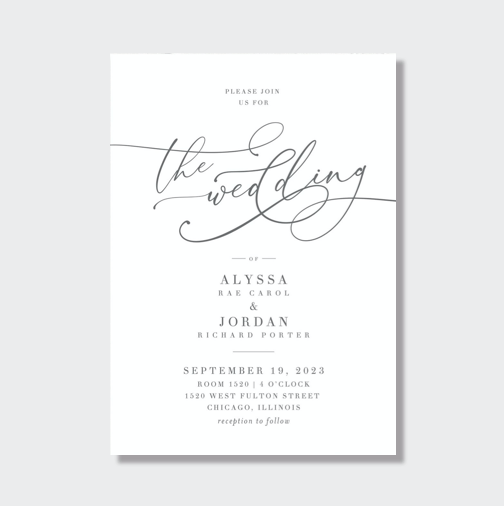
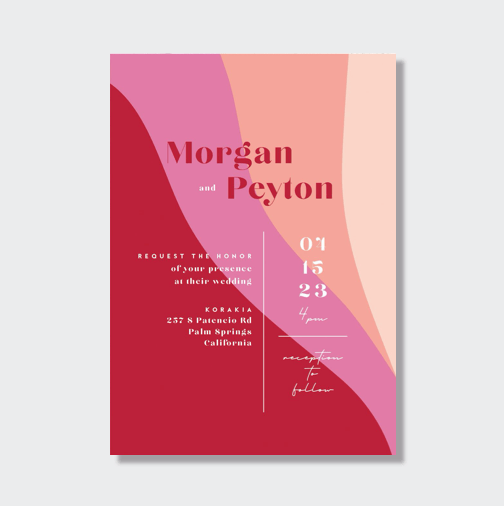
Invitations
Shop by category Get a free sample kit
- Shop
-
More
Featured registry brands
Featured designers